no
jo


hi
hellp
asd
asd
Fighting Genetics: Victory Over Hereditary Heart Disease
Hereditary heart disease can feel like an unavoidable fate, a shadow cast by family medical history that looms over one's future. However, modern medicine and proactive lifestyle choices have transformed this narrative from a predetermined sentence to a challenge that can be effectively managed and overcome.
The Genetic Landscape of Heart Disease
What Makes Heart Disease Hereditary?
Genetic predisposition to heart disease involves:
- Inherited gene mutations
- Familial cholesterol disorders
- Genetic markers for heart inflammation
- Inherited structural heart abnormalities
Key Genetic Risk Factors
- Family history of early heart attacks
- Inherited high cholesterol conditions
- Genetic variations affecting heart muscle
- Predisposition to hypertension
Strategies for Genetic Resilience
1. Comprehensive Genetic Testing
- Advanced DNA screening
- Identifying specific genetic markers
- Understanding personal risk profile
- Early intervention planning
2. Personalized Medical Approach
- Tailored medical OLE777 interventions
- Precision medicine techniques
- Targeted pharmaceutical treatments
- Regular cardiovascular monitoring
Lifestyle Interventions: Overriding Genetic Risks
Nutrition Strategies
- Anti-inflammatory diet
- Omega-3 rich foods
- Low saturated fat intake
- Antioxidant-rich nutrition
- Personalized nutritional plans
Exercise Protocols
- Cardiovascular conditioning
- Strength training
- Stress-reduction exercises
- Personalized fitness regimens
- Heart-specific workout designs
Stress Management
- Mindfulness practices
- Meditation techniques
- Psychological counseling
- Stress reduction strategies
- Emotional resilience building
Medical Technologies Transforming Genetic Challenges
Advanced Diagnostic Tools
- Genetic risk profiling
- Advanced imaging techniques
- Predictive cardiovascular modeling
- Non-invasive screening methods
Emerging Treatment Innovations
- Gene therapy approaches
- Personalized medication
- Regenerative medicine
- Targeted genetic interventions
Success Stories: Triumph Over Genetic Predisposition
Case Study: Sarah Thompson
- 42-year-old professional
- Family history of heart disease
- Proactive genetic management
- Successful prevention strategy
Case Study: Michael Rodriguez
- Inherited high cholesterol
- Comprehensive lifestyle transformation
- Medical intervention
- Reversed genetic risk trajectory
Psychological Aspects of Genetic Heart Disease
Emotional Resilience
- Understanding genetic risks
- Developing positive mindset
- Building mental strength
- Overcoming genetic anxiety
Support Systems
- Family counseling
- Support groups
- Professional psychological support
- Community resources
Practical Action Steps
Immediate Recommendations
- Conduct comprehensive genetic testing
- Develop personalized health plan
- Regular medical consultations
- Implement lifestyle modifications
- Continuous health monitoring
Financial Considerations
Managing Healthcare Costs
- Insurance coverage strategies
- Preventive care investments
- Long-term health planning
- Cost-effective screening methods
Conclusion: Empowerment Over Genetics
Genetic heart disease is not an unbreakable curse but a challenge to be understood, managed, and ultimately overcome. With advanced medical knowledge, proactive strategies, and personal commitment, individuals can significantly reduce their genetic risks and lead healthy, fulfilling lives.
Key Takeaways
- Genetics is not destiny
- Proactive management is crucial
- Lifestyle plays a significant role
- Hope and science can transform health outcomes
#GeneticHealthJourney #HeartHealthAwareness #MedicalInnovation
Disclaimer: Always consult healthcare professionals for personalized medical advice.
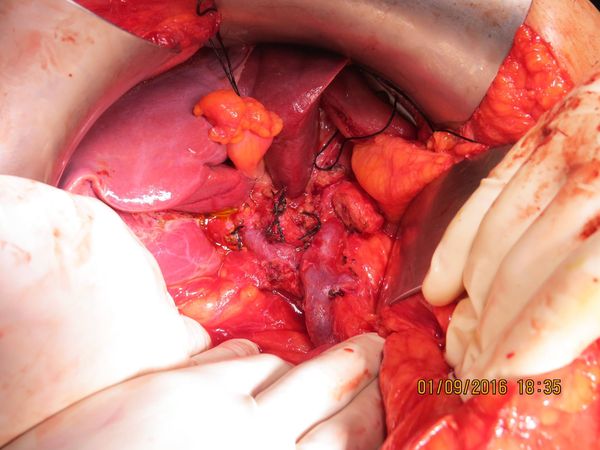
Gallbladder cancer & Myasthenia gravis
Cancer warrior: 67 yr old teacher with gallbladder cancer & Myasthenia gravis. The radical cholecystectomy was challenging mainly due to peri-operative challenges due to the Mysthenia - a condition characterised by rapid fatigue and weakness of voluntary muscles. But with excellent perioperative multi- disciplinary care by our surgical, Neuro and Anaethesia team - pt recovered well is now cancer free at 4.0 yr follow up.
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube


Cadaver Liver Transplant
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube
Bile duct cholangioca
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube


Morbid obesity ( weight 106 kg ), uncontrolled diabetes
Mrs SB aged 62 years with morbid obesity ( weight 106 kg ), uncontrolled diabetes and large recurrent ventral hernia with 2 failed previous repairs. We performed Mini gastric bypass - weight came down to 62 kg in 8 months with resolution of diabetes. Subsequently she underwent Abdomnal wall reconstruction and component separation with abdominiplasty. She is doing well 1 yr after surgery. In addition to its beneficial effects on comorbidities, bariatric surgery is now considered mandatory in morbidly obese patients with hernias to prevent reccurance.
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube
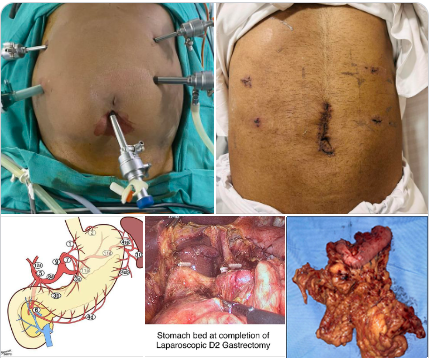
Laparoscopic D2 Gastrectomy for gastric cancer
Laparoscopic D2 Gastrectomy for gastric cancer with specimen retrieval thru a 3 cm periumbical incision. In addition to less postoperative pain the faster recovery ensures patient is ready for chemotherapy by end of second week. Delay in starting adjuvant chemotherapy after cancer surgery has major impact on long term outcomes.
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube

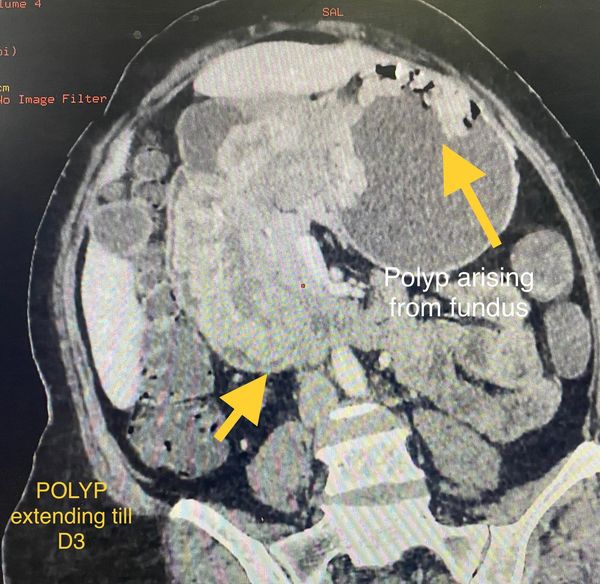
A complex pancreatic surgery : CANCER WARRIOR
Mr NB age 62 y underwent Whipples pancreaticoduodenectomy with portal vein resection ( a complex pancreatic surgery) for advanced cancer of head of pancreas followed by chemotherapy. At 4yrs follow up he remains cancer free with an excellent quality of life and still continuing with a full time job.
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube
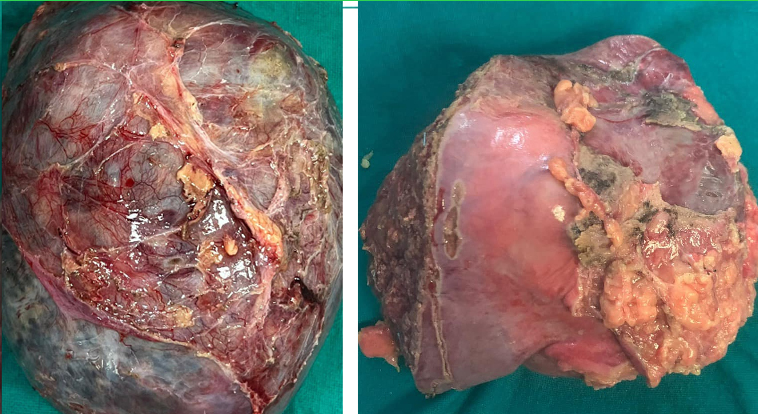
Gallbladder cancer :CANCER WARRIOR:
Ms RS aged 55 yrs underwent a radical cholecystectomy with enbloc colectomy for gallbladder cancer which is one of the most aggressive GI cancers. Post op chemotherapy and 6 years follow up later she leads an active lifestyle and remains cancer free which is equivalent to a complete cure.


Pace hospitals team successfully completed 100 BARIATRIC SURGERIES
With 3 Bariatric surgeries ( 2 MGB and one sleeve ) last week Pace hospitals team successfully completed 100 BARIATRIC SURGERIES with minimal morbidity , zero leak rates and zero mortality. Our 100 th patient was our units typical high risk patient at weight 180 kg and BMI 62 -super obese category. He presented with DM , COPD and obesity related cardiac failure for which he was on ventilator. After treating him with diuretics and weaning off ventilator to BiPaP gradually to room air. Our ICU and anesthetist team did a marvellous job of optimising him and getting him to table within 2 weeks . He underwent a sleeve Gastrectomy ( as a first part of his 2 stage surgery in view of his high risk) and had a smooth recovery. Many thanks to surgical, Anaesthesist, physcian , dietician, Physio, ICU teams for their tremendous contributions in reaching this landmark
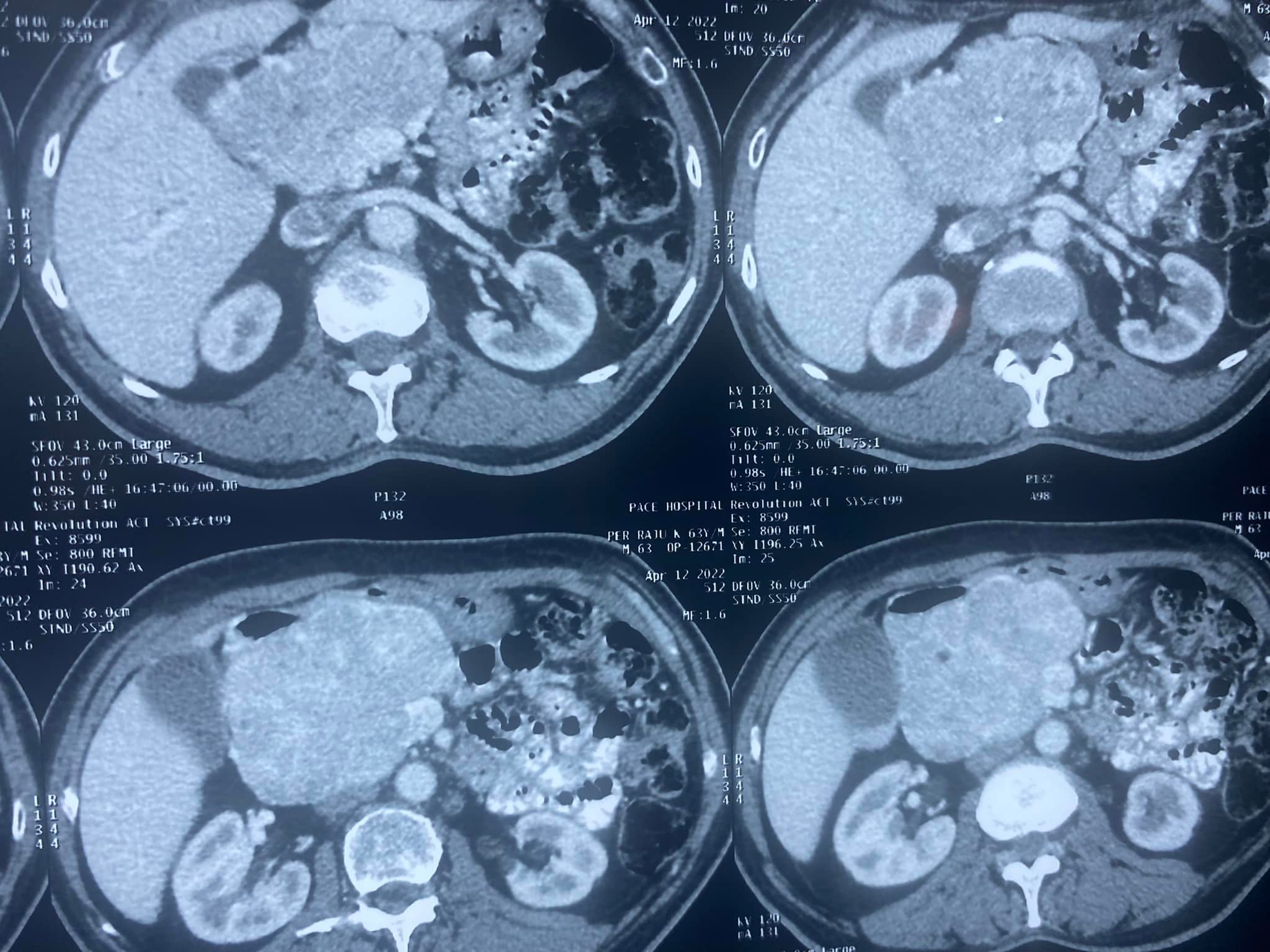
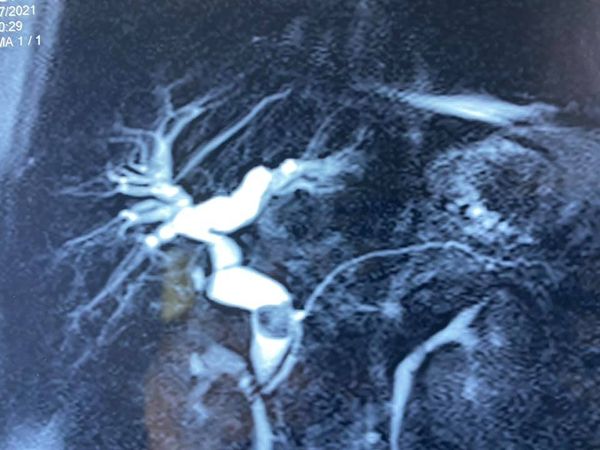
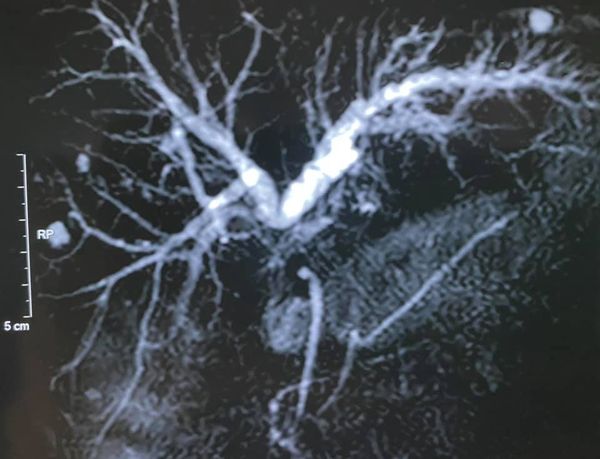
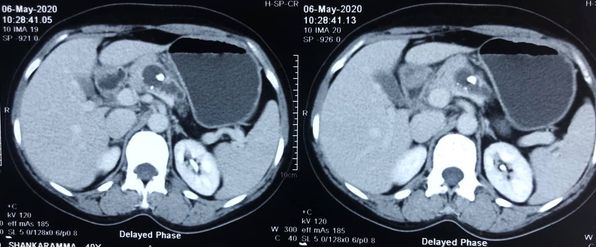
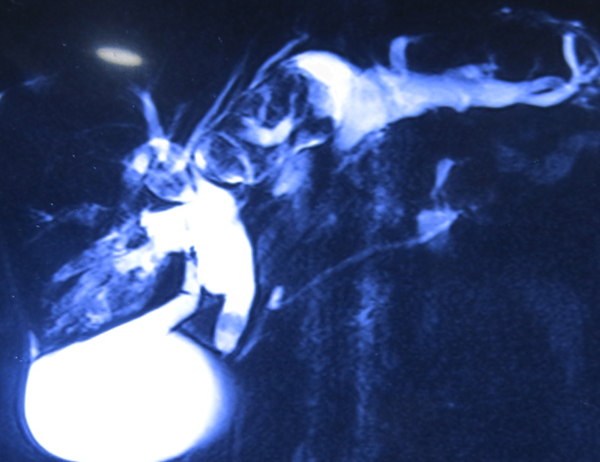
Stent blocks, stent migration , segmental cholangitis
Preoperative biliary drainage in malignant Hilar strictures with PTBD or ERCP is fraught with high incidence of problems of stent blocks, stent migration , segmental cholangitis, abscess and peri PTBD leaks so much that most patients never reach the operative table becoming ‘biliary cripples’. There is clear evidence that preop biliary drainage may be harmful in periampullary but it was considered Mandatory for hepatectomy. There is now enough evidence to demonstrate that in high volume centres atleast left sided resections can be safely done with out biliary drainage in presence of jaundice without cholangitis. This is our second such pt 60 year old with intrahepatic cholangiocarcinoma with Type 3 B block and bilirubin 14 mg %. He underwent a left hepatectomy with caudate lobectomy and bile duct excision. Hepaticojejunostomy was performed to 3 ducts on a right side. Patient had a very smooth recovery and is fit for adjuvant chemo 2 weeks after surgery. This would have been very much delayed with our normal protocol of preop biliary drainage of Rt anterior and posterior and 3 weeks waiting causing all the biliary sepsis issues .
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube

Donor Liver transplant patient
Our first living donor Liver transplant patient at Pace hospital Madhapur premises completes 1 yr today uneventfully . He is back in his job and normal life for past 9 months. The Pace team together with Dr.Madhusudhan’s team have completed 25 liver transplant combined this year at Pace , Pratima , Osmania and SMS Jaipur.
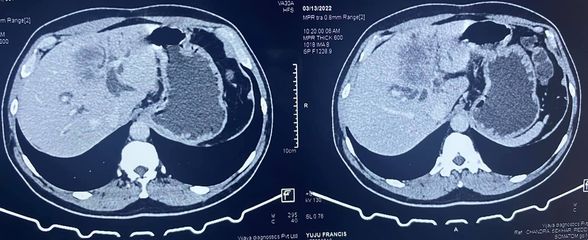
isolated polyp of stomach
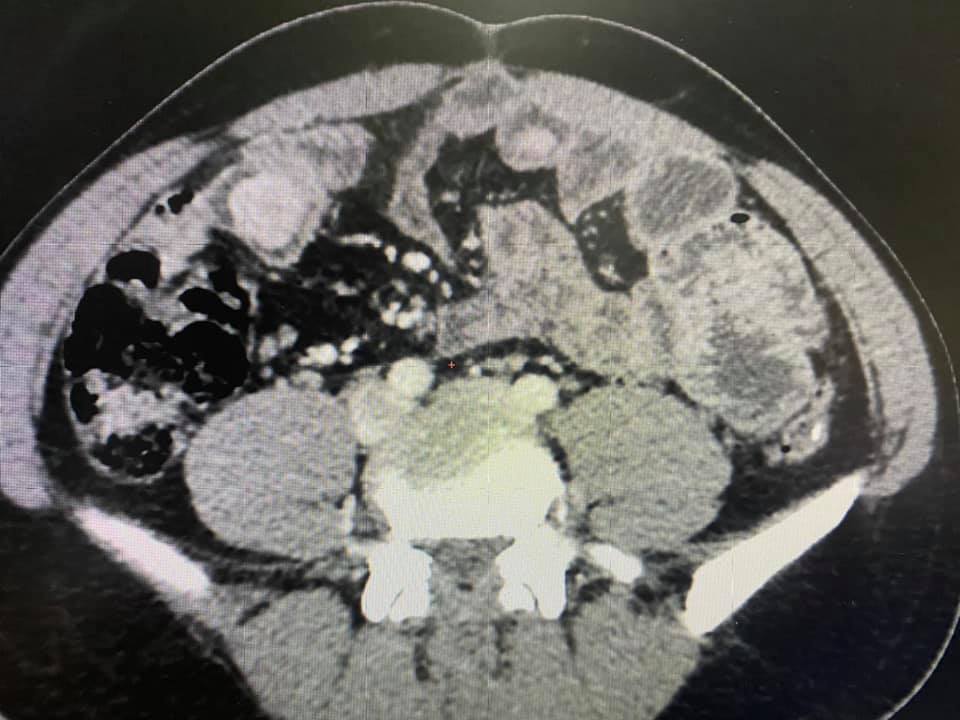
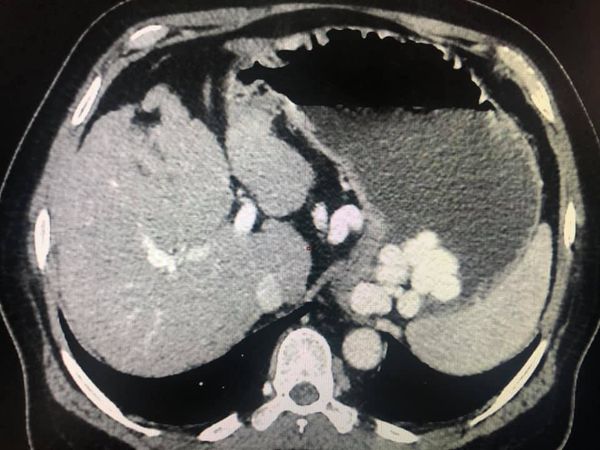
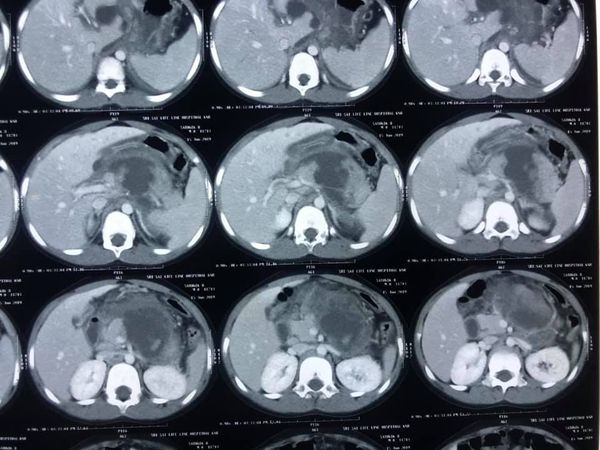
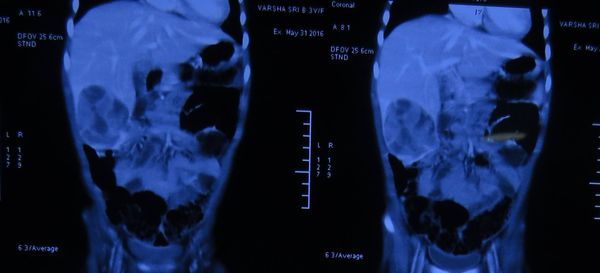
Rare and unusual case of isolated polyp of stomach causing gastroduodenal Intussesption with gastric outlet obstruction. CT images show a polyp arising from fundus of stomach prolapsing to duodenum extending till D3 D4 junction. Biopsy was inconclusive but from our previous experience these prolapsing polyps are almost always non malignant. The lack of muscle infiltration allows funneling Intussesption of stomach. Patient underwent a greater curve gastronomy reduction of gastric funelling Intussesption followed by a sleeve Gastrectomy protecting GE Jn with a boogie. Postoperative histology shows puetz -Jeghers polyp. No evidence of small bowel or colonic polyps on CT enetroclysis and colonoscopy appears to be an isolated puetzjeghers polyp of stomach. Genetic testing results are awaited
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube
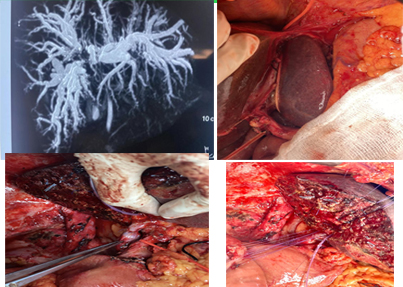
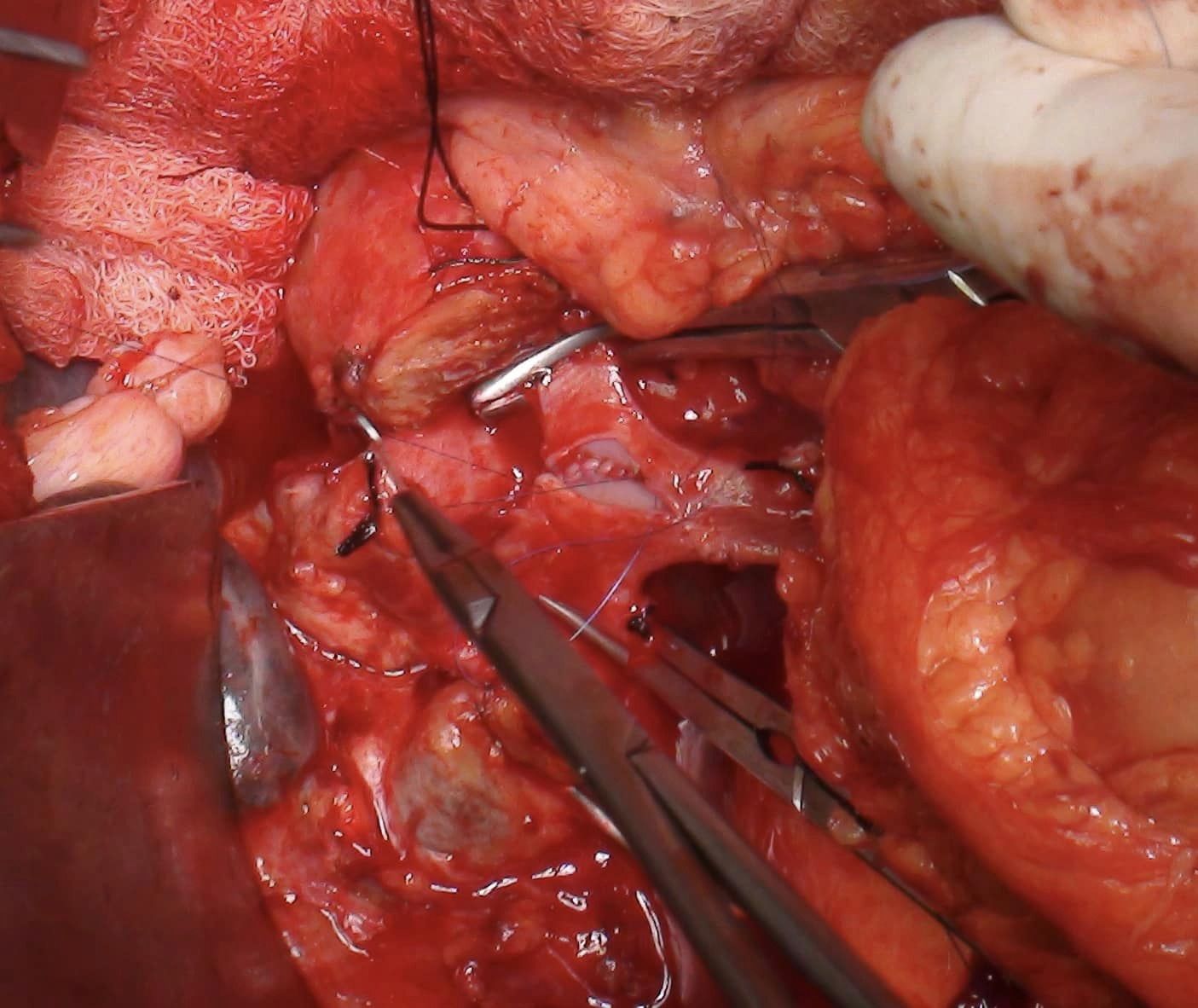
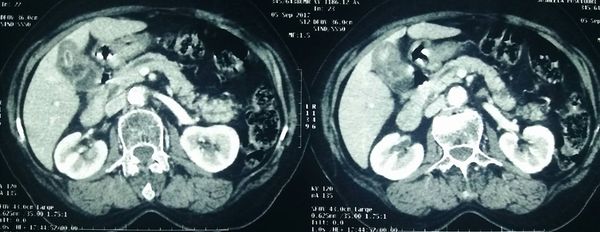
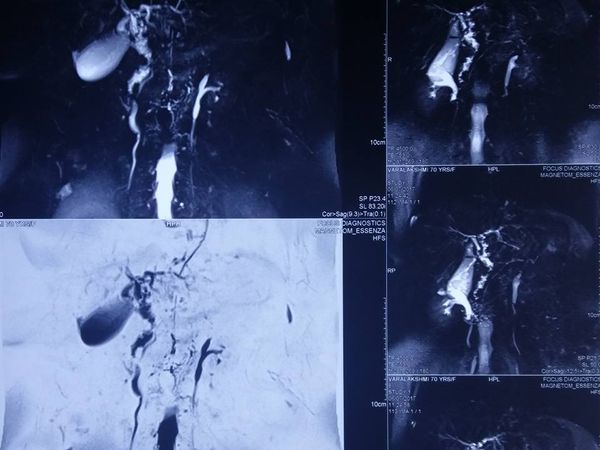
Type 3 A Hilar cholangiocarcinoma.
Type 3 A Hilar cholangiocarcinoma. Underwent left PTBD followed by extended Rt hepatectomy with caudate lobectomy bile duct excision and left portal vein segmental resection anastomosis. Similar to the long left hepatic duct allowing good bile duct margins for right sided resections the left portal vein also has a longer length and extrahepatic course allowing for technically simpler portal vein resection when needed . As it’s not feasible to differentiate peritumor desmoplasia seen in hilars from actual infiltration it’s preferable to resect the portal vein in doubtful cases to achieve -ve Circumferential margins. The left sided hanging manoeuver illustrated in Pic 2 is a useful tip to avoid injury to MHV/ LHV trunk during complete caudate resection.
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube
Laparoscopic liver resection for biliary cystadenoma
Laparoscopic liver resection for biliary cystadenoma @ Pace hospitals- using Enseal for parenchymal transection and endoGIA stapler white reload for left hepatic vein and glissonian pedicle control.
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube

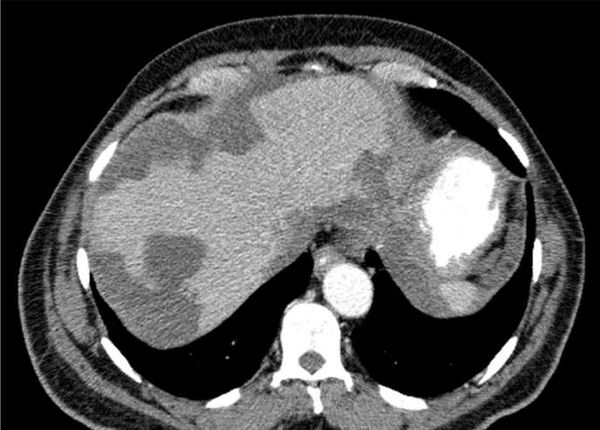
Hemmorgagic complications of liver tumor
whipples with PV resection .
whipples with PV resection . In course of whipples PD- portal vein resection of the SMV- PV confluence involves need to ligate splenic vein with it attendant complications . One way to preserve the splenic vein is to remove a sleeve of portal vein with subsequent suturing leaving opposite wall intact . However sleeve can lead to kinking of PV, narrowing and angulation torsion issues during repair with risk of postoperative thrombosis. This is a simple variation of the sleeve by which can do a segmental resection anastomosis avoiding angulation , narrowing of anastomosis while simultaneously avoiding ligation / reimplantation of splenic vein.
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube

Esophageal cancer : Cancer survivor
Mrs RS aged 62 years underwent neoadjuvant chemo-radiation followed by a thoracoscpic Esophagectomy for esophageal cancer with our team 7 years ago. She is cancer free at 7 years and declared cured from esophageal cancer (the 5 yr rule) with a completely active life style .With newer neoadjuavant protocols , multimodality care and minimally Invasive surgery outcomes and cure rates are improving in these previously dismal cancers.
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube
Vascular Resections
HPB surgery combined with vascular resections are the most complicated areas of GI cancer surgery giving gratifying results in these difficult scenarios. It was a very satisfying week of complex HPB surgery at PACE HOSPITALS with three portal vein resections - one Main portal vein resection with Whipples for 8 cm giant SPEN in a high risk Pt with 35 % Ejection fraction and- an Extended Right hepatectomy and segmental portal vein resection for Type 3 A - An extended left hepatectomy with resection of portal vein confluence for Type 3 B Hilar cholangiocarcinoma respectively. Topped by a challenging central hepatectomy. The Whipples Pt and central hepatectomy pt were discharged by day 7 and both the Hilar cholangiocarcinoma pts are recovering smoothly.
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube

Whipples Pancreaticoduodenectomy
Bile duct exploration

Liver transplantation
Idiopathic chronic pancreatitis
Colon cancer
Liver transplant


Pancreatic cancer
Gallbladder cancer

Hepatectony for liver cancer
Type lll post cholecystectomy BBS with external biliary fistula
Reccurant episodes of abdominal pain
Advanced colon cancer


Type 3 B hilar cholagiocarcinoma
Chronic pancreatitis

Stage IV neuroendocrine tumor underwent a total gastrectomy
A hilar cholangiocarcinoma
Atypical giant hemangioma
Chronic pancreatitis

Liver transplant
CLD with HUGE gastric varices
Multiple biliary polyps
Distal pancreatectomy
Recurrent cholangitis
Distal pancreatectomy with splenectomy for large pancreatic tumors
In large pancreatic tumors (such as SPEN, Mucinous tumors) where the
access to splenic vessels is not possible the antegrade approach allows safe
surgery without risk of injury to the major vascular structures i.e celiac ,
common hepatic artery and the SMV portal vein axis. The GDA is divided and
pancreas is transacted at neck to expose the junction of splenic vein with SMV
portal vein axis . Likewise the common hepatic artery is dissected till celiac
origin and then traced onto splenic artery. so that the celiac and hepatic
arteries are safegaurded in the distorted vascular anatomy by large tumor size.
Only after dividing the pancreas and then dividing the splenic vessels at the
origin safeguarding the CHA and SMV -PV axis the the resection can proceed antegrade
along the prerenal fascia to achieve medial to lateral resection. For
adenocarcinoma we proceed in same fashion but posterior to the anterior fascia
(Radical antegrade modular pancreatico splenectomy-RAMPS approach)
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube
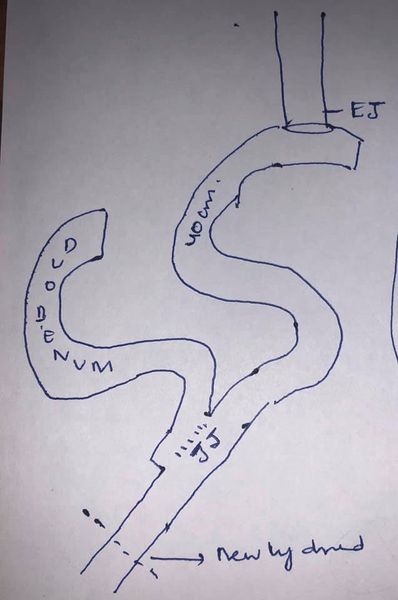
Succesful Revision of failed LPJ depends on careful case selection
Succesful
Revision of failed LPJ depends on careful case selection. Not every patient
having persistent pain after LPJ can be resolved by revision. Only patients
with reccurant pain and imaging suggestive of - inadeqately drained PD in body
tail and /or inadequate coring of head with significant ductal stone load will
respond to revision surgery. In this case- CT scan reveals mostly undrained
duct in body and tail with stricture and stone at neck and PD disruption at
neck. Like wise the jejunal limb stops at the neck indicating the head is
completely undrained. After dismantling
the anastomosis only pinhole opening in PD (6)is seen showing severe stenosis
of an already small anastomosis. The entire PD is laid open with head coring
and a 12 cm anastomosis is achieved (7-11)The previous jejunojejunostomy is
retained. We have done 4 revision LPJ in such very carefully selected patients
with excellent results. This case also illustrates the importance of doing a
wide drainage of duct and head coring during LPJ as a short anastomosis may
have temporary relief but will inevitably stricture in long run.
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube
Reccurant severe post prandial central abdominal pain

Gastric Cancer
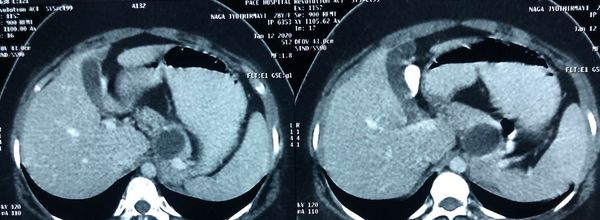
Miraculous story of a blessed 60 year old from Siddipet who presented to us with advanced gastric cancer involving pancreas and spleen. Advanced gastric cancer ( poorly differentiated variety) has a traditionally poor prognosis with a median survival of 3 to 6 months . After inserting a tube to feed her we followed a strategy of 4 cycles of neoadjuvant (preoperative ) chemoradiation to which she responded beautifully . Subsequently we proceeded with a total gastrectomy with distal pancreatectomy and spelnectomy. Biopsy revealed a near total response to the chemotherapy. She is doing great 5 years after surgery with no evidence of reccurance which is equivalent for her to a complete cure. God bless her with a long and healthy life.
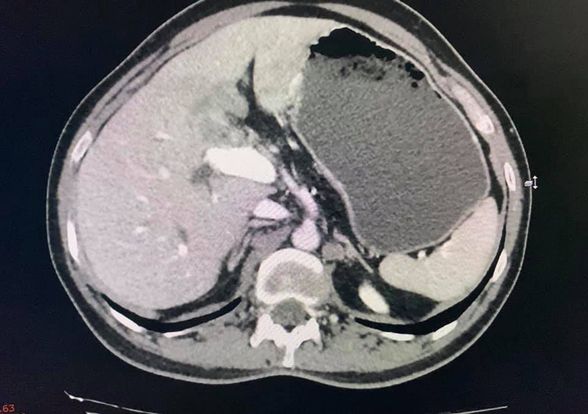
Grade 2 fatty liver Disease
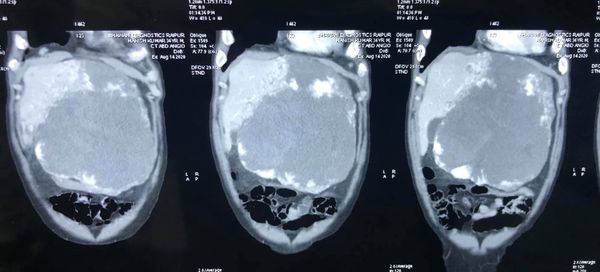
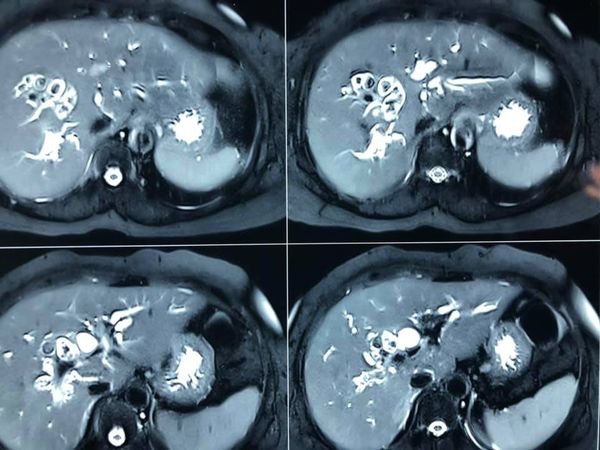
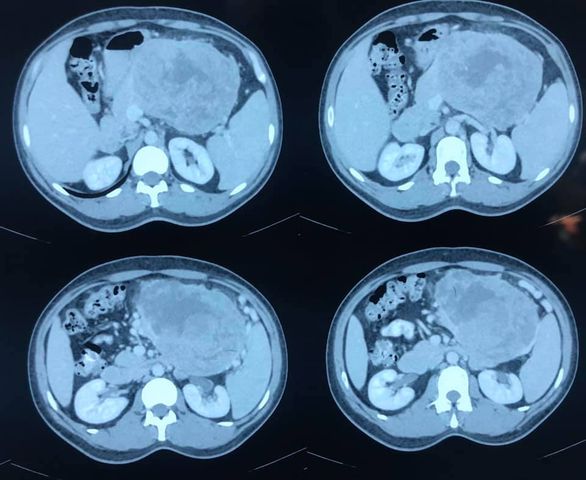
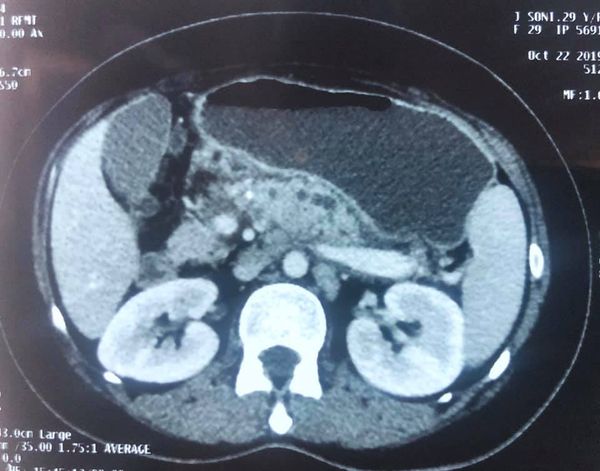
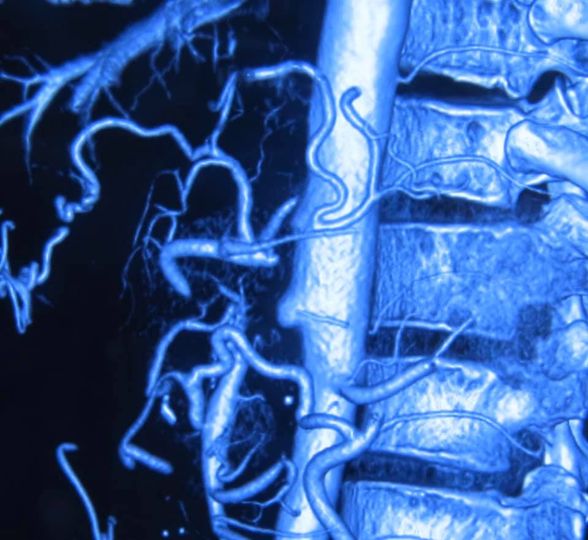
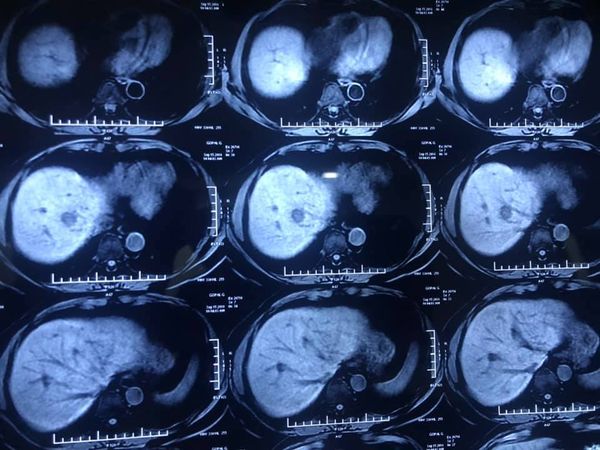
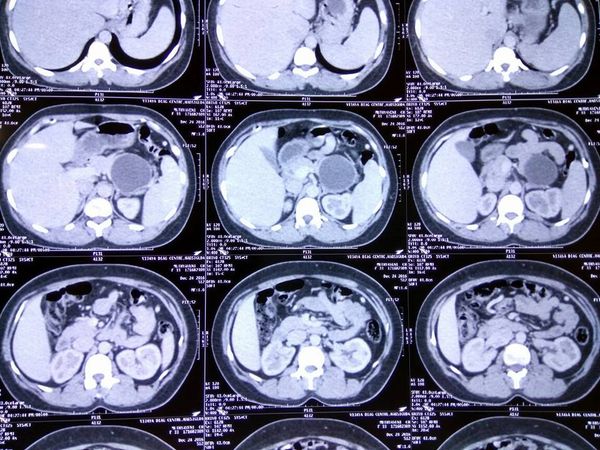
70 year old Kenyan male with grade 2 fatty liver with a 6cm HCC in segment 5 of liver. Normal LFT and no evidence of portal HT /cirrhosis. In view of the age , steatotic liver and central location of tumor he was planned for a central hepatectomy. Images show the central location of tumor in CT and MRI. The right anterior sectoral pedicle being isolated and clamped
Causing demarcation of rt anterior (seg 5 and 8 ) from right posterior ( seg 6 and 7) . The MHV being divided. The remnant liver with preserved rt posterior and left lateral segments . The central hepatectomy specimen showing tumor on cutsection . In our series of 6 central hepatectomies in diseased livers peak bilirubin has been 3.0 mg% with only one morbidity of bile leak in a patient and zero mortality (Results presented at AHPBA 2018) . These parenchyma preserving procedures allow safe hepatectomy in elderly with disease livers.
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube


Type 3 B hilar stricture and extending into bile duct
An unusual case of biliary cystadenocarinoma with papillary adenocarcinoma leading Type 3 B hilar stricture( involving secondary ducts in left side) and extending into bile duct . Patient underwent an extended left hepatectomy including Caudate lobe resection and bile duct t excision . hepaticojejunostomy was done to Rt anterior and Rt posterior ducts after a ductoplasty . intraop picture show the bileduct distended with tumor and left sided complete mobilisation of caudate lobe off IVC with control of common trunk of LHV and MHV. cut section shows the papillary tumor and the tumor extension into Lower bile duct . Caudate resection is mandatory in hilar tumors due to close approximation of the caudate lobe with Hilum as well as early tumor involvement of caudate bile ducts by hilar tumors.
Pancreatic transection
Grade 3 pancreatic injury causing complete pancreatic transection in mid-body of pancreas. In this kind of complete disruption seen on CT scan there is no possibility of bridging the gap with an ERCP stenting. Even if the patient is hemodynamically stable without bleeding. This leads to a isolated pancreatic syndrome in which the distal pancreatic secretions have nowhere to go leading to the cycle collections, pseudocyst , sepsis, pseudoaneuryms and if patient survives strictures duct in distal pancreas leading to chronic pancreatitis in the remnant. This patients with such a wide disruption and isolated pancreas are better served by a distal pancreatectomy at the initial presentation to avoid late complications.

Type 3 B hilar cholangiocarcinoma
Gallbladder cancer
Gall bladder cancer with node positivity and bile duct involvement (causing Jaundice) is considered a lost cause and dealt with in a nihilistic approach. Still for lack of better options aggressive resectional surgery followed by adjuvant chemotherapy remains the mainstay in this cancer. This 50 year old lady underwent a radical cholecystectomy with 4B /5 liver resection and bile duct excision with us 3 years ago. It was followed by post op chemotherapy. Now 3 years later she remains cancer free. Since most reccurances occur within first 2 years on gallbladder we are very hopeful of achieving a complete cure in her.

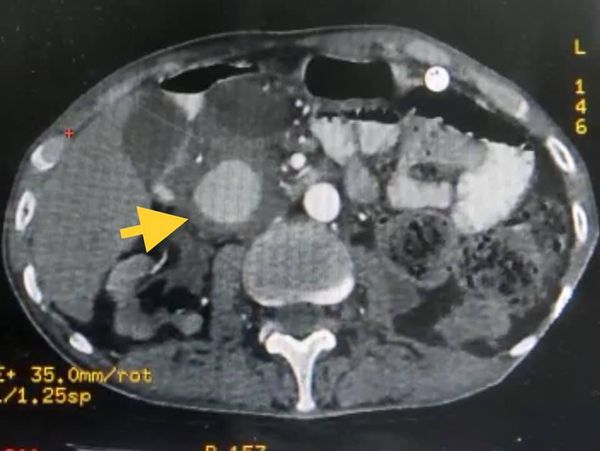
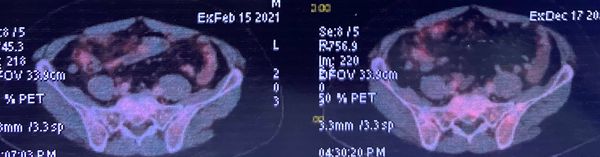
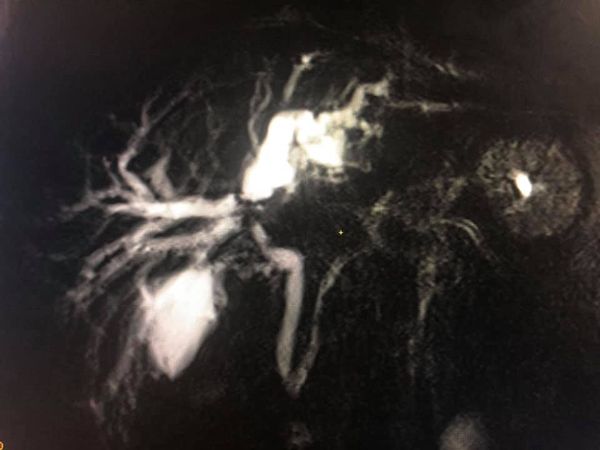
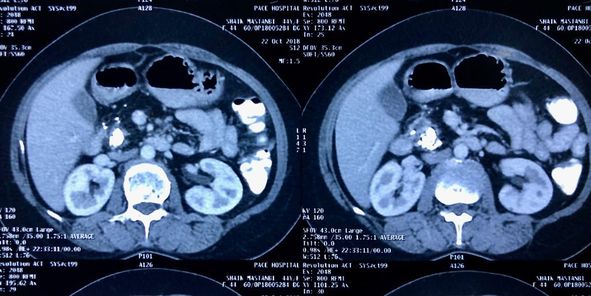
carcinoma rectum with synchronous colorectal metastasis
Major hepatectomy in borderline liver- 68 yr old male carcinoma rectum with synchronous colorectal metastasis. Patient underwent RT followed by LAR and 8 cycles of chemotherapy. Post chemotherapy MRI and PET CT shows 5 mets in Right lobe with involvement of MHV (MRI Image 1 &2) In view of age , post chemo changes in liver on imaging ) , MHV involvement and 32 % remnant volume we decided for right portal vein embolisation. PVE deprives the nutrition to right half of liver causing hypertrophy of the future remnant liver .Post embolosation liver volume increased from 370 to 520 ( approx 35% increase) At surgery the liver showed post chemochanges but due to preop embolisation we could go ahead with an extended right hepatectomy including full MHV. Using a water jet dissection we could transect the diseased liver bloodlessly without using inflow occlusion (video) Patient had ascites post op but resolved and discharged by day of 10. This case illustrates the role of PVE in improving safety of Hepatectomy in borderline /diseased livers
Type 4 choledochal cyst with hepatolithiasis underwent resection
28 year old girl Type 4 choledochal cyst with hepatolithiasis underwent resection of extrahepatic choledochal cyst 6 years ago with duodenal access loop else where. She presented to us 2 years after surgery with persisting symptoms with reccurent epioses of pain with jaundice and cholangitis. 3 ICU admissions in septic shock. Out side attempted endoscopic interventions through duodenal access and PTBD did not relieve symptoms. When we saw the patient her MRI and CT scan images showed multiple cholangiolytic abcess with large stones in the left lobe . On imaging Majority of stones were in the Left lobe and with a few stones inthe right posterior segment wheras the right anterior segment was completely disease free. Traditionally the approach for bilateral hepatolithiasis would a transplant with attended risk in a septic patient and cost. in view of segmental disease we tried a different approach. After stabilising for 2 weeks on antibiotics we took her up semi electively for left hepatectomy for left sided disease and intraoperative choledochoscopy of right posterior segment calculi .after clearing all stones we placed an intraoperative retrograde PTBD in R post segment to promote better drainage and did a 3 cm revision HJ to the right duct. Patient has bile leak from cut surface post op but subsequently settled. Rt PTBD was removed after 1 year. 4 years later the patient is completely symptom free and Check CT (image) shows no residual stones. This way we successfully avoided the risk of a potential liver transplant in a septic patient with excellent longterm results

Whipples Resection
This 12 yr old
young man is one of our youngest Whipples ( the youngest being 8 years old) .
He presented with a rare childhood tumor called solid papillary tumor of
pancreas 8 cm in size with the portal vein (main blood vessel of liver) splayed
out over it. In view of vascular involvement he was told be a very high risk
for surgery in Vijaywada and came to us. We did a technically challenging
Whipples resection with a portal vein reconstruction 6 months ago. Doing great
postoperatively, Recent he received a letter that that he has been selected for
a NASA scholarship for 2 weeks and came to me for a fitness certificate. A very
lively and jovial fellow.. I asked him if he wants to be a GI surgeon- he could
come and work with me later. His reply-“ No thanks. I see you always in
tension. I’d rather become an astronaut”. God bless him with a long and
plentiful life.
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube
Liver Cancer surgery
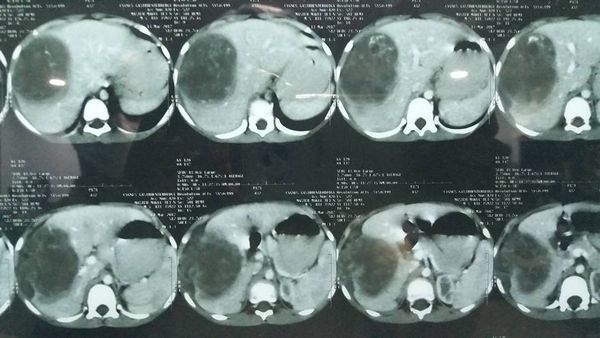
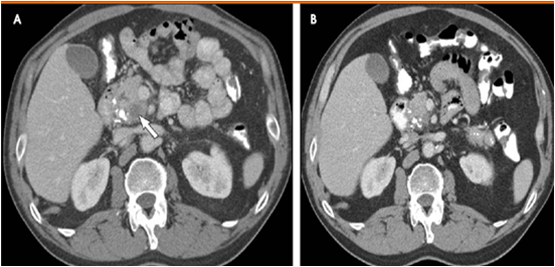
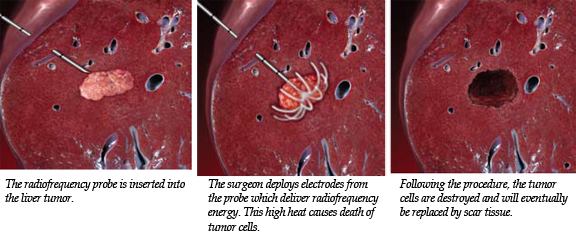
MICROWAVE ABLATION - AN IMPROVED TOOL FOR INOPERABLE HCC : 68 year old HCV positive male child’s B presented with 3x 3 cm HCC ( primary liver cancer ) in seg 1 and 5 of liver , 1 year after a previous laparoscopic surgery by us for 2 cm seg 2 HCC. Traditionally these lesions in Seg 1 of liver were not fit For RFA ( radiofrequency ablation) due to the heat sink effect from the neighbouring blood vessels . However microwave ablation uses electromagnetic waves to cause oscillation of water molecules causing frictional heating and tissue necrosis. It overcomes traditional disadvantages of RFA Which relies on impedance. It has been shown to achieve quicker , more complete ablation with better tumor response than RFA. Patient has been advised listing for transplantation.


Liver Cancer surgery
MICROWAVE ABLATION - AN IMPROVED TOOL FOR INOPERABLE HCC : 68 year old HCV positive male child’s B presented with 3x 3 cm HCC ( primary liver cancer ) in seg 1 and 5 of liver , 1 year after a previous laparoscopic surgery by us for 2 cm seg 2 HCC. Traditionally these lesions in Seg 1 of liver were not fit For RFA ( radiofrequency ablation) due to the heat sink effect from the neighbouring blood vessels . However microwave ablation uses electromagnetic waves to cause oscillation of water molecules causing frictional heating and tissue necrosis. It overcomes traditional disadvantages of RFA Which relies on impedance. It has been shown to achieve quicker , more complete ablation with better tumor response than RFA. Patient has been advised listing for transplantation.
carcinoma rectum with solitary liver metastasis
Cancer survivor: 70 yr old Mr R from east Godavari had carcinoma rectum with solitary liver metastasis which is actually stage IV disease . Traditionally stage IV cancer has extremely poor outcomes with survival in months. But by careful selection even stage 4 rectal cancer can be treated with a curative intent. Despite many people advising to contrary he put his trust in us and underwent a LAR (rectal cancer resection) with a liver resection 4 years ago. Today he came in for his annual check up before permanently migrating to Australia where his 2 kids reside. After the tests I cleared him as disease free at 4 years( 5 yrs equivalent to cure) and we shared this happy picture . May god bless him with a long and healthy life.

Idiopathic chronic calcific pancreatitis
Reccurant pyogenic cholangitis
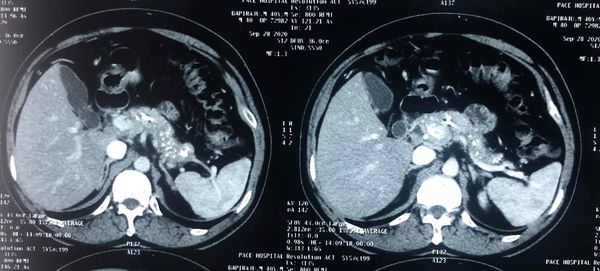
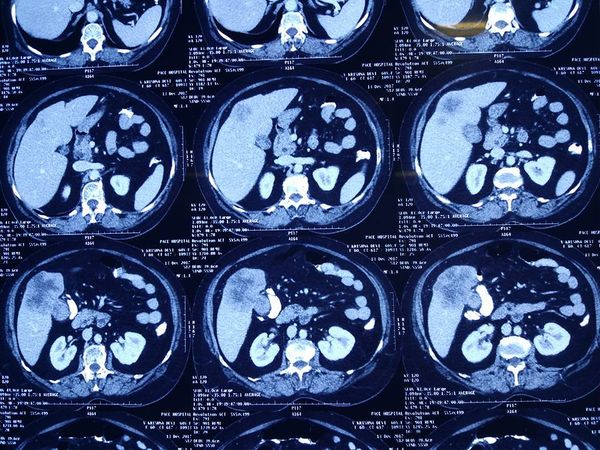
Interesting images September: Reccurant pyogenic cholangitis (RPC) 67 yr old Bangladeshi lady presented with reccurant episodes of jaundice fever and pain for past 1 year. MRCP and CT scan showed left duct stricture with left sided IHBRD and CBD stones and atrophy of left lateral segment. As she 4 duct was also involved we did a left hepatectomy with hepaticoduodenostomy . Reccurant pyogenic cholangitis is a disease charecterised by multiple instances of biliary bacterial infection, hepatic abcesses , multiple stricturing of bile ducts with pigment stone formation in the intrahepatic and extrahepatic biliary tree. This can cause reccurant episodes of cholangitis, chronic illness ultimately leading to liver failure. It is more common in the far east population. Management includes long term biiary drainage with liver resections for segmental disease and liver transplantation in patients with end stage liver failure . The last CT scan shows another similar patient with huge intrahepatic stones and abscesses managed successfully by surgery and long term PTBD.


Liver Cancer survivor
Pancreaticoduodenectomy with splenectomy
Interesting images June: Total pancreaticoduodenectomy with splenectomy done for a 45 yr female with main duct IPMN with invasive mid-body cancer with bilateral polycystic kidneys. Her EUS, ERCP and fluid cytology , fluid CEA , serum CA19 -9 were all suggestive and a PET showed high uptake in her solid component .She is doing well post op but planned for adjuvant CT Rt as tumor had breached capsule and encased splenic vein. Total pancreaticoduodenectomy was previously frowned upon as a high morbidity surgery due to severe exocrine and endocrine insufficiency with brittle diabetes , and ulcerogenicity due to complete loss of pancreatic bicarbonate secretion. But in recent years with easy availability of enzyme supplements, CGM ( continuos glucose monitoring devices), insulin pens and long acting PPI the long term QoL of these patients is comparable with partial pancreatectomy patients


Liver cancer survivor
Liver cancer survivor: This 72 yr old gentleman came came for follow up after liver cancer surgery 4 years ago. At that time due to his age and small liver remnant he was told to be incurable by other centres but by using a special complicated technique called ALLPS ( first time in my career) we performed a safe surgery and here he is 4 years later with a healthy liver remnant and no evidence of recurrence.After a high risk surgery with all its attendent stress its extremely gratifying have such a pleasing result.
RESECTION WITH HIPEC CHEMOTHERAPY FOR PSEUDOMYXOMA

VASCULAR ANAMOLY DURING HPB Surgery.
Peritoneal disease on laparoscopy
Carcinoma GB large fundal growth with (suprisingly) no LN mets on PET and no peritoneal disease on laparoscopy. We did a radical cholecystectomy with seg 4B and seg 5 with extended lymphadenectomy of hepatoduodenal , retropancreatic, common hepatic and celiac LN. Cutsection shows growth limited to fundus with extensive liver infiltration.Once there is no M stage disease and no celiac or aortocaval lN involvement... for fundal growth.If its minimal infiltration we do 2 cm wedge...more extensive such as this patient we do a 4B and 5. However once growth involves the neck and cystic duct Rt hilum of liver is involved and a formal extended Rt hepatectomy with bileduct excision. However most such patients resectability rates and survival are poor. Hopefully this is one with good biological behaviour.

Liver cancer
80 yr old male 10th day after hepatectomy for Rt lobe HCC(liver cancer) . No one looking at him will believe he is 80. Irequested to share his story to inspire us. The general tendency among people including cancer specialists is to write off patients based solely on advanced age. But like i keep repeating age is just a number. Every patient needs to assessed induvidually. A 60 yr may not be fit for a haircut while a 90 yr old may be fit for a whipples or liver resection (as was the case last year with one of our patients). its the physiological age and frame of mind which matters more than the chronological age. And this is not just in hepatobililiary surgery but in every aspect of life.
Carcinoma gallbladder
Carcinoma gallbladder- 67 yr old lady with polypoidal mass growing gradually over past 3 years. undewent a radical cholecytectomy with 2 cm liver wedge and extended lymphadenectomy of hepatoduodenal, retropancreatic, common hepatic and celiac LN. biopsy revealed papillary adenocarcinoma with no LN involvement. papillary Ca GB has a better prognosis compared to the more common infiltrative variant where resctability rates and outcomes are poor.fundus and proximal body masses may be treated 2 cm wedge or segment 4b and 5 resection while neck masses infiltratate the hilum early , presnt with jaundice and need major liver resections with biliary reconstructio. and poor survival rates.
Major Liver Resections
Spyglass cholangioscopy

5 yr Cancer survivor
50th PANCREATIC CANCER RESECTION IN 2 YEARS:

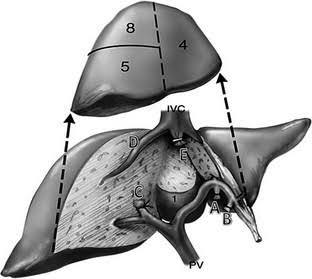
60 year old male with HCV related well compensated CLD
Interesting case: 60 year old male with HCV related well compensated CLD , Childs A status with normal platelets and no varies on endoscopy. presented with HCC invoving segment 4 5 and 8 As we see in imaging option was Rt trisectionectomy which would have been too risky. As right hepatic vein was free.we performed central hepatectomy in which segment 4 5 and 8 are removed presercing the right posterior segment are preserved.In this unique parenchyma preserving operation the segment 4 and RT anterior pedicure are divided by glissonian approach and MHV is divided.RHV is preseved by CUSA dissection. there by despite central location of tumor enough parenchyma is preserved for safe recovery.it's a very rare and complex surgery only my 3rd in 10 years.
Gastric cancer.
Cystic neoplasms of pancreas
Hydatid cyst of liver

colectomy with resection
A brave heart who underwent a colectomy with resection of solitary liver metastases for colon cancer at a ripe 84 years and lived to tell 5 years later. Touching 90 but still young and playful at heart she is one of my favourite patients. No one will believe she's 90.
Chronic pancreatitis (CP) and maliganancy
Advances in Liver surgery
Extended whipples for ductal adenocarcinoma

Pancreatic cancer surgery
Liver metastases indicates stage IV disease
Cancer spread to liver is not always
the end of the road !
In Gastrointestinal or No GI
malignacies (ovary,uterus, breast etc) the presence of liver mestastases
indicates stage IV disease with poor survival. Neurendocrine tumors (and
colorectal cancers) are an exception to this rule. Patients with neuro endocrine
tumors have good 10 and 20 yr survival rates especially the well differentiated
cancer. This was a patient with a neuroendocrine type I gastric tumor with
spread to lymphnodes and a solitary liver metastasis who underwent a
gastrectomy (removal tumor bearing stomach) with a D2 Lymphadenectomy (very
extnesive lymphadenectomy) and non anatomical resection of liver metastases. We
expect an excellent long time survival in this patient despite stage IV
disease. other modalities like RFA of liver metasases and Trans arterial
chemoembolisation are available for these patients now.
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube

Liver Resection
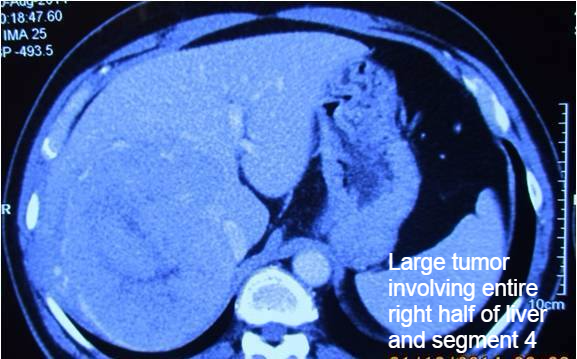
2 year girl with rare childhood liver tumor sucessfully managed with a major liver resection
Hepatoblastoma is a rare childhood tumor which usually occurs in children younger than 3 years of age. It is usually managed by surgery with chemotherapy before or after surgery. gita was a 2 yr old child with tumor involving right half of liver with elevated alfa fetoprotein suggestive of hepatoblastoma. Most of these patients usually present in a more advanced stage and are managed by chemotherapy followed by surgery. In case of gita tumor was involving on 4 out of 8 segments of liver so she was planned for a primary surgery. followed by chemotherapy. She undewent a surgery in which approximately 65% of liver was removed with the tumor. Post operative recovery was smooth. Kudos to the anaesthesist and critical care team for helping us accomplish this rare surgery in a young child.
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube
A UNIQUE PANCREAS PRESERVING OPERATION
Central
pancreatectomy involves removal of only the tumor bearing portion of pancreas
after meticulously separating it from vessels. The distal pancreas is preserved
in contrast to the standard distal pnacreatectomy for students. This leads to
better preservation of exocrine and endocrine function. If expertise in
pancreatic surgery is available this operation in selected patients of cystic
pancreatic neoplasms allows a better quality of life after surgery.
Postoperative recovery was smooth. Biopsy revealed a serous cystadenoma of
pancreas which has excellent longterm outcomes.
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube




