WHAT ARE THE CRITERIA FOR PATIENTS CONSIDERING SURGERY FOR OBESITY OR BARIATRIC SURGERY?
Obesity is very difficult to treat. Many patients have tried multiple diets, medications and exercise regimes that had results that did not last. Surgery to promote weight loss by restricting food intake and interrupting digestive processes is an option for clinically severe obese patients that have been unsuccessful with other weight loss treatments.
Weight loss surgery may also be an option for people with a BMI of 35 or greater who suffer from progressive life-threatening obesity related health problems such as diabetes, obesity-related heart disease or severe sleep apnea. However, as is true for other treatments for obesity, successful results depend significantly on knowledge, personal motivation and behavior.
How does surgery promote weight reduction ?
Bariatric surgery produces weight loss by restricting food intake and, in some cases, interfering with nutrition through malabsorption. Patients who undergo bariatric surgery must also commit to a lifetime of healthy eating and regular physical activity. These healthy habits help ensure that the weight loss from surgery is successfully maintained.
What are the surgical options ?
There are four types of operations that are commonly offered: adjustable gastric band (AGB), Roux-en-Y gastric bypass (RYGB), biliopancreatic diversion with a duodenal switch (BPD-DS), and vertical sleeve gastrectomy (VSG). Each has its own benefits and risks. To select the option that is best for you, you and your physician will consider that operation’s benefits and risks along with many other factors, including BMI, eating behaviors, obesity-related health conditions, and previous operations.
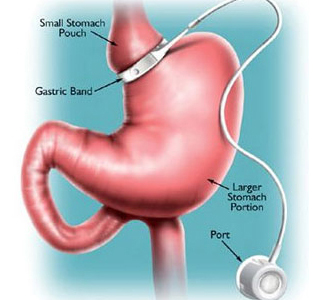
Adjustable Gastric Band
AGB works primarily by decreasing food intake. Food intake is limited by placing a small bracelet-like band around the top of the stomach to produce a small pouch about the size of a thumb. The outlet size is controlled by a circular balloon inside the band that can be inflated or deflated with saline solution to meet the needs of the patient.
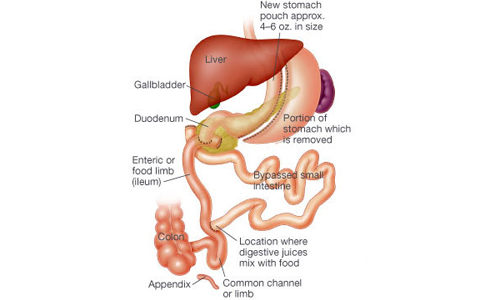
Roux-en-Y Gastric Bypass
RYGB works by restricting food intake and by decreasing the absorption of food. Food intake is limited by a small pouch that is similar in size to the adjustable gastric band. In addition, absorption of food in the digestive tract is reduced by excluding most of the stomach, duodenum, and upper intestine from contact with food by routing food directly from the pouch into the small intestine.
Biliopancreatic Diversion With a Duodenal Switch
BPD-DS, usually referred to as a “duodenal switch,” is a complex bariatric operation that principally includes 1) removing a large portion of the stomach to promote smaller meal sizes, 2) re-routing of food away from much of the small intestine to partially prevent absorption of food, and 3) re-routing of bile and other digestive juices which impair digestion. In removing a large portion of the stomach, a more tubular “gastric sleeve” (also known as a vertical sleeve gastrectomy, or VSG) is created. The smaller stomach sleeve remains connected to a very short segment of the duodenum, which is then directly connected to a lower part of the small intestine. This operation leaves a small portion of the duodenum available for food and the absorption of some vitamins and minerals. However, food that is eaten by the patient bypasses the majority of the duodenum. The distance between the stomach and colon is made much shorter after this operation, thus promoting malabsorption. BPD-DS produces significant weight loss. However, there is greater risk of long-term complications because of decreased absorption of food, vitamins, and minerals.
Vertical Sleeve Gastrectomy
This is the most preferred bariatric surgery. The sleeve gastrectomy is a surgery only on the stomach (it is only a restrictive procedure) and does not involve any surgery on intestine (which would make it malabsorptive).. It basically consists of making a stomach into a long tube; therefore the name “sleeve”. The sleeve gastrectomy (SG) removes two-thirds of the stomach, which provides for quicker satiety (sense of fullness) and decreased appetite. The smaller stomach pouch restricts food intake by allowing only a small amount of food to be eaten at one time. After the separation of the stomach into small tube, the remainder of the stomach is removed. The valve of the outlet of the stomach remains, this provides for the normal process of stomach emptying to continue which allows for the feeling of fullness. There is no malabsorption. There is no dumping syndrome. The Sleeve Gastrectomy is believed to have an advantage over the Adjustable Gastric Band due to removal of the part of the stomach that produces the hormone (Ghrelin) that controls the desire to eat. The potential complications of the operation on average are typically less than 0.5% compared to 2%-3% in a combined procedure.
WHY CHOOSE THE SLEEVE GASTRECTOMY?
The sleeve gastrectomy has the following advantages
- It does not require the implantation of a foreign body such as a silastic ring used in gastric banding.
- The procedure mechanically decreases the size of the stomach but also decreases the secretion of the hormone ghrelin which is responsible for the feeling of satiety (fullness).
- The procedure offers the benefit of initially decreasing the body weight in the severely obese patient to prepare this patient for a staged procedure or other surgery at a later time.
BENEFITS
The medical and emotional benefits of weight loss procedures begin almost immediately after surgery. Over time, the benefits may include:
- Significant weight loss
- Improvement of Type 2 diabetes.
- Lower blood pressure.
- Lower cholesterol
- Relief of sleep apnea
- Relief of acid reflux
- Decreased joint pain, improved mobility
- Improved mood and self-esteem
RISKS
Weight loss surgery, as with any major surgery, has risks of which you should be made aware: These may include:
- An internal infection from leakage of digestive juices into the body cavity
- Wound infections at incision sites
- Development of gall bladder disease and / or gall stones – due to rapid weight loss
- Blood clots – may cause a more serious condition called a pulmonary embolism
- Vitamin deficiencies – may be preventable by taking daily vitamin supplements. Periodic lab testing may also be required
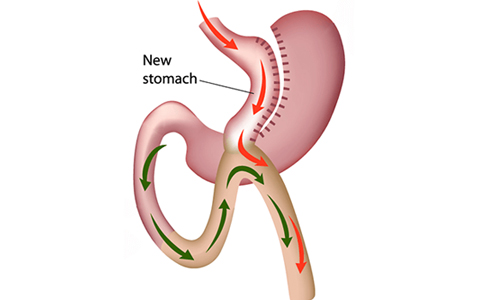
Mini Gastric Bypass Surgery
Laparoscopic Mini Gastric Bypass which is also called as one anastomosis gastric bypass as well as omega loop gastric bypass or modified Billroth II procedure. In this the Gastric pouch is like a long sleeve which is anastomosed (joined) to the intestines, making a loop thereby finishing the procedure with only single anastomosis.
It has a theoretical advantage over RYGB in causing no intestinal obstruction in long term follow up. The results of excess weight loss and resolution of co morbidities is similar to that of RYGB. This procedure is primarily a malabsorptive procedure as compared to the classical RYGB.
The patient has a better capacity and tolerance to quantity of the food but as it causes more malabsorption the frequency of stools may be increased. Post MGB, we have seen brilliant results in special subtype of our population.
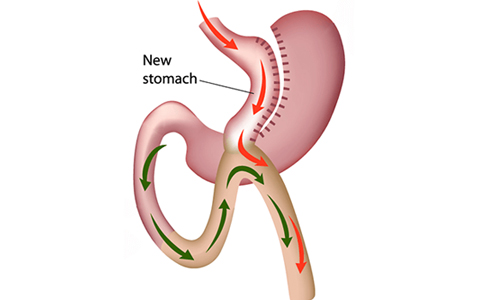
Sleeve gastrectomy with proximal jejunal bypass
It is a new procedure to treat obesity and type 2 diabetes. In this procedure first laparoscopic sleeve Gastrectomy is done. After that jejunum (a part of small intestine) is divided 50 cm from the ligament of treitz. 200-300cm of proximal jejunum is bypassed and end to side jejunojejunostomy is done.