Advanced Pancreatic NET with Portal Hypertension: A Surgical Success Story
30 yr old male with Locally advanced pancreatic NET with celiac encasement and portal vein thrombosis with portal cavernoma with extensive collaterals. He has been managed by biliary stenting for past 6 yrs . His metallic SEMS blocked despite multiple interventions and patient has been going around for a solution recurrant cholangitis but was refused because of high risk. He has not been jaundice / pruritis free for past 3 yrs. he presented to to us with metallic stent within stent blocked with cholangitis and bilirubin 23mg %. After initial biliary decompression and a 3 week waiting period .We performed splenectomy with splenorenal shunt to decompress the portal hypertensive collaterals followed by a hepaticojejunostomy and gastric bypass. The NET is non progressive for 6 yrs and will be managed by lantreotide. From our previous experience with HJ in EHPVO the lesson we have learnt is if the target organ (bile duct) is dilated > 1.5 cm and the stricture is low (Type1 or 2) - HJ can be safely attempted by experienced HPB surgeons. The pattern and distribution of collaterals ( anterior/ vs posterior, intramural ) also needs to mapped Pre operatively to help in decision making and approach.


Extended central hepatectomy
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube
Vascular reconstruction
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube
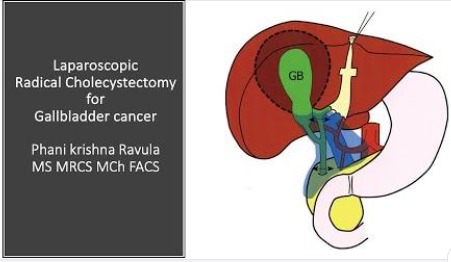
Laparoscopic Radical Cholecystectomy for gall bladder cancer
Step by step technique of Laparoscopic Radical Cholecystectomy for gall bladder cancer. Teaching videos of Seg 4B,5 resection for and extent of liver resection in gallbladder cancer are available elsewhere in our channel ( links in endscreen)
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube
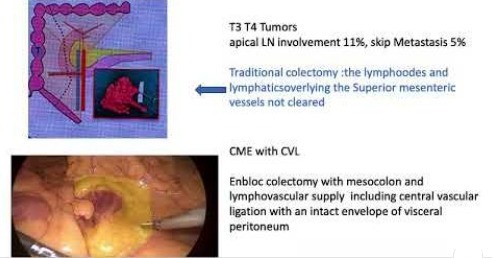
COMPLETE MESOCOLIC EXCISION with CENTRAL VASCULAR LIGATION
This video describes step by step technique of COMPLETE MESOCOLIC EXCISION with CENTRAL VASCULAR LIGATION( CME with CVL) in extended right hemicolectomy for carcinoma Transverse colon. Tips for safe dissection of root of transverse mesolon at origin of gastrocolic & middle colic trunks with diverse anatomical variations is also discussed.
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube
GLISSONEAN approach to liver resection
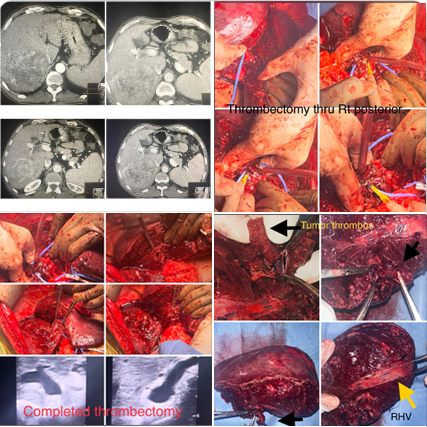
Illustrating advantages of GLISSONEAN approach to liver resection avoiding extrahepatic dissection . 62 yr old male HBV CLD Childs A with well preserved liver function with Segment 6,7 HCC with tumor thrombus in Rt portal vein till confluence .Rt anterior portal branch and MPV were free ( CT images ) Patient was planned for a parenchyma preserving Rt posterior sectionectomy with tumor thrombectomy. In the traditional approach extrahepatic manipulation & dissection of Rt portal vein and clamping would risk rupture of tumor thrombus and migration. Therefore we went ahead with a glissonean approach avoiding dissection of extrahepatic Rt portal pedicle. Rt posterior sectionectomy was performed isolating Rt posterior Glissonean pedicle (without clamping) & using RHV as for parenchymal trasection. At the last step portal inflow control was achieved by simple pringles applied at hepatoduodenal ligament . Glissonean pedicle was divided ( without clamping) as last step of specimen removal and a controlled thrombectomy thru the Rt portal vein orifice could be achieved without clamping or dislodgement of tumor thrombus. Ontable doppler confirmed complete clearance of the tumor thrombus from the confluence with patent Right anterior hepatic vein , MPV & LPV. Post operative recovery was uneventful.
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube
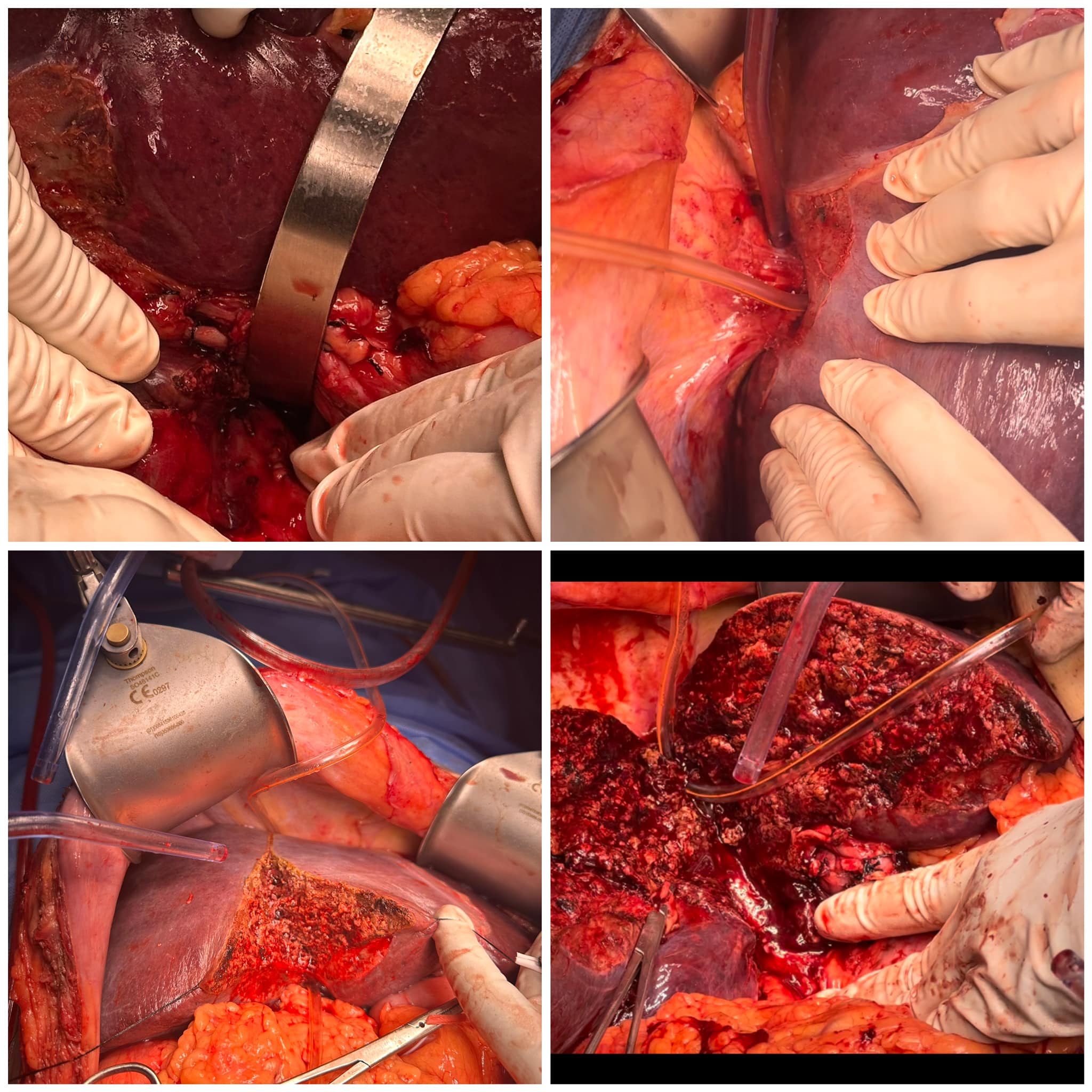
Exophytic right lobe HCC with hepatic vein thrombus extending across Ostia into IVC.
Anterior approach , no touch technique for hepatectomy : 72 yr old male with exophytic right lobe HCC with hepatic vein thrombus extending across Ostia into IVC. There is risk of tumor rupture and thrombus migration during right lobe mobilisation using traditional technique. In the anterior no touch technique the hanging manoeuver is achieved by retrohepatic precaval tunelling without right lobe mobilisation and handling. The hanging facilities safe transection. The anterior surface of IVC is exposed ,the right hepatic vein is controlled & tumor thrombus is removed using no-touch technique. Only after this right lobe mobilisation done by dividing the short hepatics , Makucchi ligament and other retroperitoneal attachments.
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube
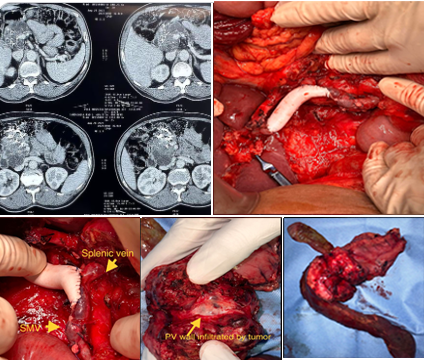
Main Duct IPMN whipples with portal vein resection and reconstruction with PTFE graft.
Main duct IPMN whipples with portal vein resection and reconstruction with PTFE graft. For tumors involving the PV- SMV junction , If only medial wall is involved (less than 180 degree) keeping common ostia of splenic and SMV simplifies the reconstruction. Despite portal vein resection, with careful perioperartive planning Patient was on a fast track recovery discharged by day 5. If vein at SMV PV confluence is more than 270 degree involved then splenic need to be ligated or reconstructed separately.
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube
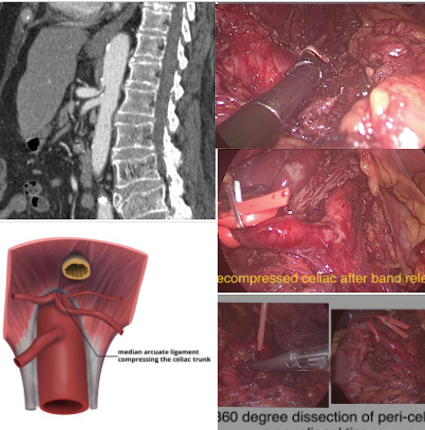
Median arcute ligament compression
Median arcute ligament compression is a frequent incidental finding in CT scan. Symptomatic patients are selected after meticulously ruling out other causes -by UGIE , CT, MRCP , EUS even rarer causes like biliary & papillary dyskinesia, porphyria , vascular causes . In 15 yrs we have selected only 6 cases where we felt that clinical symptoms, radiological findings - post-stenotic dilatation and high flow velocities, complete work up to exclude other causes favoured a diagnosis of MALS. In our limited experience and review of literature the laparoscopic treatment of MALS includes not just release of arcute compression of celiac axis as is usually done. A meticulous and complete excision of all the ganglionic tissue around celiac origin 360 degree is also vital for optimal relief. Older detailed video of technique is available at our channel.
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube

post radical cholecystectomy for gallbladder cancer
Large subcostal blowouts post open chole & HPB - transplant surgeries are one of the most challenging hernias to manage due to wide gaps ,subcostal retraction of muscle and multiple defects. This was one such our own patient post radical cholecystectomy for gallbladder cancer 3 yrs back. The Modified TAR involves a superior release till posterior aspect of diaphragm laterally & central diaphragmatic tendon till IVC medically. Inferior & lateral extent release is done as per standard TAR. The midline dissection is ‘modified ‘to stay in preperitoneal plane avoiding retrorectus dissection as midline advancement is not needed. Two 30x 30 prolene meshes are placed . Postoperative recovery was uneventful.
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube
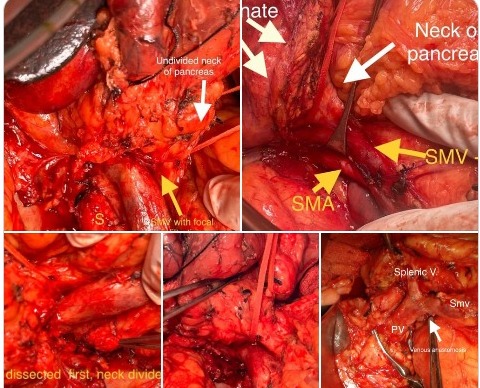
SMA artery -first approach to Whipples PD
Two recent cases illustrating the “SMA artery -first approach “ to Whipples PD . The traditional advantages of dissecting the uncinate first off the superior mesentery artery 1. helps confirm resectability in borderline resectable Ca HOP before any irreversible steps, 2. Helps get better CRM at uncinate translating to better onco logical outcomes. Additional advantages in our experience- 3. In patients with SMV PV resection helps in doing enbloc resection as last step with immediate reconstruction and avoiding bowel congestion ( as posterior dissection is already done) 2. Minimal to no blood loss from the already devascularised head and uncinate during neck transection which is done very late in SMA first. In traditional uncinate last whipples surgery excess oozing from head and uncinate during after transection leads to bloody field and leads to difficulty during uncinate dissection potentially leading to compromise of CRM
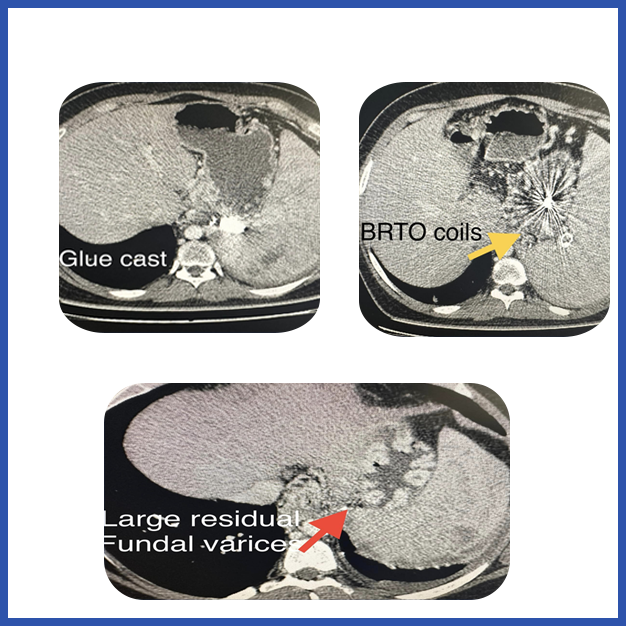
EHPVO with fundal varices and hypersplenism and transfusion induced RVD
Decades old procedure revisited - A 38 yr old male with EHPVO with fundal varices and hypersplenism and transfusion induced RVD. With reccurant gastric varices bleed despite 2 times glue injection and BRTO coiling. CT shows post glue cast, and BRTO coils with large residual fundal varices ( white arrow). Splenic vein and SMV thrombosed and unshuntable anatomy. CD4 counts persistently low despite zero viral load on antivirals ( due to hypersplenism) . In these patients modified siguira procedure involves splenectomy , gastroesophageal devascularisatuon of proximal two-third of lesser and greater curve and lower 10 cm esophagus without disturbing the porto-azygous collaterals , gastric transection at fundus body junction and pyloroplasty (as patient has a highly selective vagotomy during the devasc procedure close to the gastroesophageal wall
Linkedin | Facebook | Instagram | Twitter | Pinterest | Youtube



